Standard practice in the American healthcare system has been to monitor a patient’s blood sugar/risk for diabetes via a blood test known as the Hemoglobin A1c (HA1c). This blood test measures an individuals average blood sugar over the past 3 months and usually gets checked once or twice a year by your primary physician.
An average individual with an average American diet is commonly notified at their yearly visit that their hemoglobin A1c is normal and that they do not have diabetes. But unfortunately this info could be misleading.
Individuals with certain medical conditions can have false HA1c readings. Hemoglobin A1c is measuring the amount of glucose attached to hemoglobin (a protein in red blood cells). Since red blood cells usually survive approximately 3 months, we can get a good idea of what your average blood sugar has been over the past 3 months by looking at this lab value. Unless you have a medical conditions in which your red blood cells do not survive for 3 months. Some individuals will have decreased survival of their red blood cells (for various reasons) and therefore will have a falsely decreased hemoglobin A1c and in turn false reassurance that they aren’t at risk for diabetes.
It takes years of poor eating habits and high blood sugar spikes to produce an abnormal Hemoglobin A1c. Following a sugary meal and a spike in blood glucose, your pancreas will release insulin to bring your blood glucose back into normal range. For years your body will be able to compensate for the daily abnormal glucose spikes by having the pancreas release more and more insulin. During this time your HA1c will remain normal but your body is developing insulin resistance. Finally one day your body will become so insulin resistant that you can’t produce enough insulin to normalize blood glucose any longer. Your hemoglobin A1c will be elevated and the diagnosis of Diabetes will be made.
But even with false readings, bad eating habits and high insulin levels aside, just checking a hemoglobin A1c a few times a year is not giving an individual the full picture concerning their blood sugars.
A CGM is a wearable device that tracks your blood sugar in real time. We recommend the Dexcom G7 (prescription only) as it tracks blood sugar every 5 minutes. Dexcom also sells an over the counter version (the Dexcom Stelo) that tracks blood sugar every 15 minutes. At half the price of the G7, the Stelo is a reasonable alternative.
Because blood sugar spikes (even for a short period of time) cause damage to our blood vessels and contribute to cellular aging! Therefore, glucose optimization is a key component of health and longevity.
As blood glucose rises following a meal, glucose begins to enter your cells. The higher your blood glucose, the more glucose you have going into cells.
If too much glucose enters your cells, this causes mitochondrial overload and subsequently your mitochondria produce reactive oxygen species. Too much production of reactive oxygen species leads to inflammation, cellular damage and subsequently damage to your blood vessels. Over the long term, this leads to cardiovascular disease and aging.
Unfortunately, it doesn’t take much for production of reactive oxygen species to occur. At blood glucose levels of just 135, an individuals blood vessels can begin to get damaged.
Therefore it is crucial that individuals monitor blood glucose closely throughout the day and modify behaviors to prevent glucose spikes.

The picture above is showing the daily blood glucose for an individual over the course of a month. Each blue bar represents the blood glucose range for that particular day. For the most part, this individual consistently has well controlled blood glucose. Except for one day (red arrow) his blood glucose went much higher than any other day. So what happened?
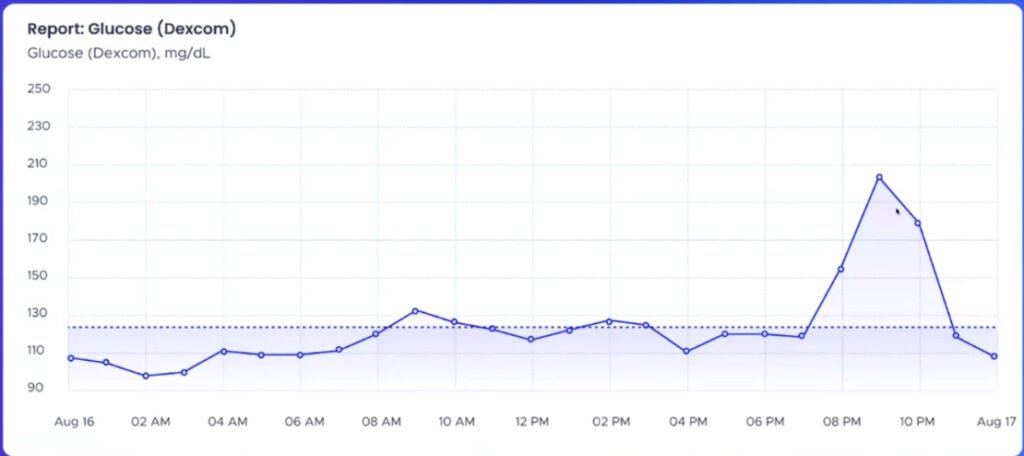
We can look deeper into that abnormal day with the graph above and see that it was a single blood glucose spike around 9pm that caused such a significant abnormality. It turns out this individual decided to eat a really large bowl of fruit that evening, not realizing it would spike blood glucose to extreme levels.
Now lets not get confused. We love fruit! And there is nothing wrong with eating fruit. But if an individual was to have a nightly fruit bowl that spiked their blood glucose to greater than 200, this would cause cellular damage and aging over the long term.
By wearing a CGM device, this individual was able to gain valuable insight into how certain foods affected their blood glucose.
Continuous glucose monitoring is powerful. It offers valuable insights into how specific foods, activities and even stress may affect glucose levels. Having this insight promotes behavioral changes that lead to lifestyle modification and gets us closer to health optimization.
This post is for educational purposes only and should not be construed as medical advice. We recommend you consult with your doctor immediately for any and all medical advice.

Follow us on social media